Rheumatoid Arthritis vs. Osteoarthritis
Arthritis is inflammation of the joints, a condition that has two main causes. Rheumatoid arthritis (RA) is an autoimmune disorder, and osteoarthritis (OA) is degeneration of the joints over time. While the underlying causes are different, there are similarities to the symptoms.
The general symptoms of both types of arthritis are painful and stiff joints, reduced range of motion of the joints, warmth or tenderness in the joints affected, and more severe symptoms first thing in the morning.
Contents
What Is Rheumatoid Arthritis?
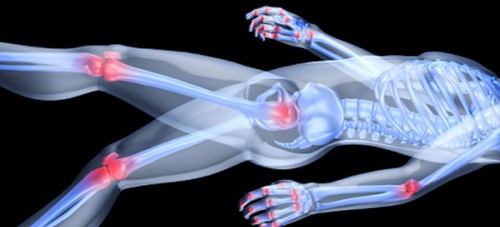
Image via Flickr by gm.esthermax
With rheumatoid arthritis, the body has an autoimmune disorder that causes it to attack itself. The immune system targets areas of your body like the soft lining in the joints, attacking it like it would fight a virus or bacterial infection. Rheumatoid arthritis causes swelling from excess fluid in the joints. The fluid accumulation causes pain, stiffness, and inflammation near the joints.
This type of arthritis can occur from childhood through adulthood. Rheumatoid arthritis has various symptoms, including joint pain, that can develop and progressively worsen over weeks or months. Onset is commonly between the ages of 30 and 60 for women, occurring later for men. It’s about one-tenth as common as osteoarthritis.
What Is Osteoarthritis?
Osteoarthritis is the most common type of arthritis and is the degeneration of the joints over decades of mechanical wear and tear. Cartilage breaks down and reduces the amount of cushion in joints. Bones eventually rub against each other, causing pain as nerves are exposed. Mild inflammation occurs, but it’s not related to an autoimmune issue. The onset of osteoarthritis is gradual over several years, but this may be accelerated by trauma to a joint. This type of arthritis affects about 27 million Americans.
Which Symptoms Are Specific to Rheumatoid Arthritis?
In addition to affecting the joints, rheumatoid arthritis can affect the entire body, causing issues in the eyes, lungs, heart, blood vessels, or nerves. The risk of heart disease is also elevated by 50%. It can result in a low-grade fever, especially for children. Rheumatoid arthritis can also cause muscle aches and excessive fatigue.
More advanced cases of rheumatoid arthritis can cause rheumatoid nodules, hard lumps under the skin near joints that could be tender. Inflammation can lead to permanent damage to the joints if it’s not managed correctly. Rheumatoid arthritis commonly appears first in smaller joints like fingers, eventually developing in knees, shoulders, ankles, and other joints. Symptoms manifest themselves symmetrically, affecting both sides of the body at the same time. While both types of arthritis commonly have worse symptoms in the morning or after an hour of inactivity, stiffness may take over an hour to subside.
Rheumatoid arthritis can be challenging to diagnose, with a variety of other symptoms in addition to joint pain.
Early diagnosis is essential, as permanent damage joint damage can occur less than one year from the onset of symptoms. Doctors may need to conduct some tests to make an official diagnosis, including blood tests and X-rays. A thorough physical exam is required to check for swollen or tender joints as well as other symptoms. Health history is also important in diagnosing rheumatoid arthritis.
Which Symptoms Are Specific to Osteoarthritis?
Osteoarthritis symptoms are limited to the affected joints, which may have an aching to burning sensation or experience sharp pain. It may lead to lumps under the skin near joints, but those spots are different than rheumatoid nodules. Osteoarthritis may result in bone spurs, which are excessive bone growth along the edges of arthritic joints.
Osteoarthritis isn’t symmetrical, so its symptoms could include pain in one knee or worse pain in one side of the body than the other. It commonly manifests itself in the hand and fingers like rheumatoid arthritis. Osteoarthritis is common in the spine, hips, and knees. Symptoms often include worse stiffness in the morning or after inactivity, but movement typically helps, and pain subsides after a few minutes. Muscles may be weakened around the arthritic joints, especially the knees. Advanced arthritis may cause joint deformation, limited range of motion, and cracking and creaking of the joints.
Diagnosing osteoarthritis is more straightforward. Doctors will inquire about the symptoms being burning, aching, or sharp. They will want to know how long the symptoms in the morning last before they subside and if there is swelling in the affected joints. Doctors will look for joint tenderness, swelling, and any weakening of muscles. Other standard diagnostic tools include X-rays to look for joint damage and blood tests to check for other conditions causing joint pain.
What Are Treatment Options?
Treatment for both rheumatoid arthritis and osteoarthritis seeks to reduce pain, improve the functioning of the joint, and minimize further joint damage. Doctors approach the two types of arthritis differently but with the same goals in mind. Both types of arthritis respond to anti-inflammatory and corticosteroid medications. Although there isn’t a cure for either type of arthritis, treatments manage the symptoms and reduce further damage from occurring.
For rheumatoid arthritis, doctors may prescribe immune system suppressants to stop the immune system from attacking joints. Treatment plans include medicine, exercise, and long-term lifestyle changes. Early treatment is key to preventing permanent damage and effectively managing symptoms. Doctors will prescribe medications and long-term management like resting when tired, using assistive devices, following a diet and exercise regimen, and staying a healthy weight. Surgery to replace joints like the knee may be required eventually.
For osteoarthritis, common treatment plans from doctors include over-the-counter pain medication such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs). Stronger prescription medication or shots of medicine in the affected joints may also be needed. Applying heat may help relax affected muscles, while ice can reduce pain and swelling. Special joint creams may also assist with pain management. Surgery like hip or knee replacement or finger joint fusion are an option if other methods are no longer effective.
While rheumatoid arthritis and osteoarthritis may have similar symptoms, the root cause of the two medical conditions is substantially different. Determining the root cause of the onset of joint pain as early as possible is essential so a care plan can help manage pain and prevent further joint damage. If you have arthritis symptoms, especially if they began appearing over a short time, contact the Hand and Wrist Institute for answers to your questions.